What is pharmacogenomics?

Pharmacogenomics is a form of personalised medicine, where the dose and type of drug given to a person is decided based on their genetic makeup.
- Pharmacogenomics is a relatively new field that combines the science of drugs (pharmacology) with the study of genes (genomics).
- It looks at how a person’s DNA affects the way they respond to certain drug treatments, to predict how effective a drug will be, at which dose, and with any side effects.
- Researchers are currently using this information to develop genetic tests and help guide decisions about which drugs an individual patient should or shouldn’t be prescribed.
What is pharmacogenomics?
- As humans, we share around 99.5% of our genomes. The remaining 0.5% doesn’t sound like much – but represents millions of genetic differences.
- Some of these genetic differences can make a person more reactive to certain medications or more vulnerable to certain diseases and conditions.
- Pharmacogenomics combines the science of drugs with our understanding of these genetic differences to help guide decisions about which medicines a person should be prescribed.
How can genomics affect the way a person will respond to drugs?
How effective the drug will be:
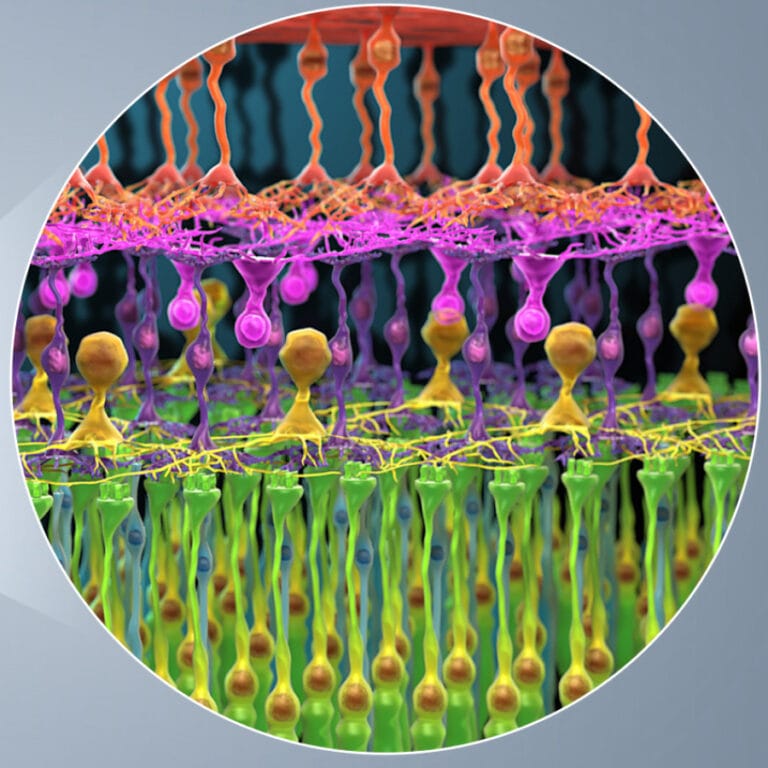
- For a drug to be effective, it needs to interact with the right cells. Genetic variations can affect the surface of a cell and influence the way it interacts with the drug.
- This information could help doctors decide if a drug will work for their patient and whether they should prescribe it.
- For example, some people’s breast cancer has extra copies of the gene HER2, which makes the cancer cells more vulnerable to a drug called Herceptin. If the cancer has low or no HER2, the drug won’t work. Doctors can use this information to decide whether to prescribe Herceptin.

The best drug dosage for them:
- Once a drug has reached the right part of the body, it is broken down and processed. Genetic variations can influence how quickly or slowly a cell can break down the drug.
- This information can help doctors decide the right dose for their patients. If the drug is processed quickly, a person might need a higher dose for it to be effective, while slow processing might need a lower dose.
- For example, doctors can test for two specific genes to predict how quickly a person’s body will breakdown the antidepressant drug amitriptyline and work out the best dosage.
The chance of serious side effects:
- The speed a drug is broken down can also influence serious side effects. If a drug is broken down very slowly or not at all, it can cause an allergic reaction.
- Doctors can now perform genetic tests to predict if a person will have a bad reaction to some drugs.
- For example, abacavir is a treatment for people with HIV, but around 1 in 17 people will have an allergic reaction. All patients now have a specific test before starting the treatment to predict if they are likely to have an allergic reaction and should not be prescribed the medicine.
Challenges of pharmacogenomics
Pharmacogenomics already plays a role in treating some diseases and is likely to be an important part of future medical care.
However, there are many obstacles for us to overcome before it becomes routine.
- Developing new tests and adhering to regulations:
- After finding a link between a genetic variant and a drug response, a suitable test must be developed and shown to be effective in clinical trials. This includes proving its usefulness and cost-effectiveness in a healthcare setting.
- Regulatory agencies also have to consider how they will assess and license pharmacogenetic products or tests.
- The complexity of genomics:
- It’s relatively rare for a particular drug response to be affected by a single genetic variation. Often, many genetic and environmental factors interact to influence a person’s response to a drug.
- This means it’s not guaranteed that a drug will or won’t be effective for someone or that a person will or won’t have a bad reaction to it.
- Integrating into healthcare services:
- Health services will have to adjust to new tests and processes. This includes new training and likely changing the behaviour of individual doctors to prescribe the right dose for their patients.
- Patients still need to follow instructions closely for a drug to be its most effective. Many side effects and ineffectiveness are caused by patients not taking medicines as prescribed.
Pharmacogenomics and new drugs
As well as optimising dose and drug type, pharmacogenomics can be used for developing new, targeted drugs. This is because some diseases are caused by specific changes, or mutations, in a gene.
This is an evolving area of research but is already making a difference for people with some types of illnesses.