What is hereditary non-polyposis colorectal cancer?
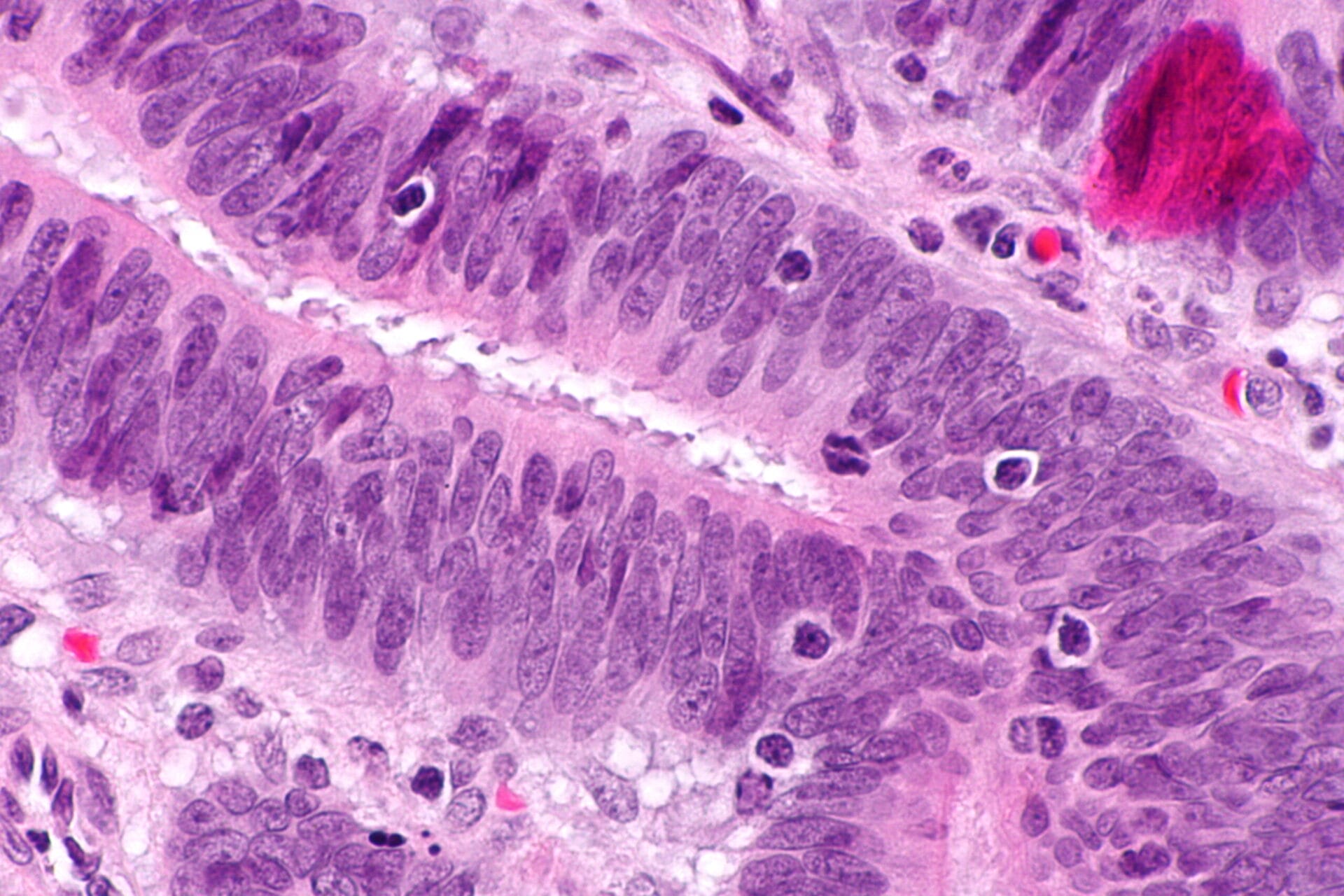
Image credit: Nephron / via Wikimedia Commons
Hereditary non-polyposis colorectal cancer is a rare condition, but it’s the most common type of inherited colorectal cancer. It’s typically caused by an inherited condition called Lynch syndrome.
- Lynch syndrome is an inherited condition that increases a person’s risk of developing certain cancers – including ovarian, stomach, small intestine, skin and brain cancers.
- When Lynch syndrome causes colorectal cancer, it’s called ‘hereditary non-polyposis colorectal cancer’.
- Hereditary non-polyposis colorectal cancer accounts for between 2 and 7% of colorectal cancer cases, making it the most common type of inherited colorectal cancer. However, across the general population, the condition is relatively rare.
What is hereditary non-polyposis colorectal cancer?
- Hereditary non-polyposis colorectal cancer is caused by an inherited genetic condition called Lynch syndrome.
- It’s often associated with mutations in a set of genes that are responsible for repairing DNA.
- These genes are the MLH1, MSH2, MSH6 or PMS2 genes, and having one mutated copy is enough to increase a person’s risk of cancer. Around 90% of cases are caused by mutations in the MSH2 and MLH1 genes.
- Mutations in the EPCAM gene can also indirectly increase an individual’s risk of developing the disorder. The EPCAM gene lies next to the gene MSH2 on chromosome 2 and some mutations in the EPCAM gene can switch the MSH2 gene off.
What is the biology of hereditary non-polyposis colorectal cancer?
- The genes MLH1, MSH2, MSH6 and PMS2 are all involved in repairing the mistakes that occur when DNA is copied in preparation for cell division.
- Mutations in these genes mean that mistakes made during DNA replication might not be properly repaired. As the cells continue to divide, they copy the mistakes over and over.
- This can then lead to uncontrolled cell growth and possibly cancer.
- However, the body is usually very good at catching mistakes made during DNA replication, so not everyone with mutations in these genes will develop cancerous tumours.
- Lynch syndrome also increases the risk of other cancer types, including ovarian, stomach, small intestine, skin and brain cancers.
What are the symptoms of hereditary non-polyposis colorectal cancer?
- Hereditary non-polyposis colorectal cancer is called ‘early onset’ cancer, with the symptoms developing at an average age of 44 years.
- It might not have any symptoms. However it can have similar symptoms to other colorectal cancers, including rectal bleeding, stomach pain and other cancer-related symptoms like unexplained weight loss and fatigue.
- Despite the name, hereditary non-polyposis colorectal cancer can cause the formation of polyps – but far fewer than seen in familial adenomatous polyposis. These polyps are generally not cancerous at first, but can become cancerous over time.
- People with Lynch syndrome have a lifetime risk of developing colorectal cancer of 15 to 80%, depending on a range of factors. This is compared to around 5% in the general population.
How is hereditary non-polyposis colorectal cancer diagnosed?
- As with other colorectal cancers, a diagnosis is usually confirmed with a colonoscopy.
- This involves a doctor inserting a small camera up the bottom of the patient to view the colon and identify the presence of any potentially cancerous polyps.
How is Lynch syndrome managed?
- People can be tested for Lynch syndrome using genetic testing to see if they have a mutation that could increase their risk of colorectal cancer. This is usually done in partnership with a genetic counsellor.
- People with Lynch syndrome will also likely be closely monitored by a specialist doctor and undergo regular reviews, including colonoscopies and screening to look for bowel abnormalities so they can be treated or removed before they become cancerous.
- The regularity of this monitoring will depend on which country they are in, how old they are and the age of onset of colorectal cancer in other members of their biological family.
- Taking a daily aspirin has also been shown to help reduce the risk of colorectal cancer in some people with Lynch syndrome.
- Some treatments are also showing promise for people whose Lynch syndrome is associated with certain mutations. This raises the possibility of personalising treatment for people they go on to develop colorectal cancer.