What is antibiotic resistance?
Antimicrobial susceptibility testing in petri dish. Image credit: Shutterstock

A major public health issue, antibiotic resistance is when bacteria develop the ability to survive exposure to antibiotics designed to kill them or stop their growth.
- Antimicrobials are medicines used to prevent and treat infections in humans, animals and plants. They include antibiotics, antivirals, antifungals and antiparasitics.
- Antibiotics are used to treat or prevent bacterial infection.
- Antibiotic resistance is when the bacteria develop the ability to survive exposure to the antibiotics that are designed to kill them.
What are antibiotics?
- Antibiotics are medicines used to treat or prevent infections caused by bacteria.
- They work by inhibiting the growth of or destroying the bacteria.
- Antibiotics work in various ways, such as destroying the bacterial cell wall or inhibiting the generation of energy from glucose within the bacterial cell.
What is antibiotic resistance?
- Antibiotic resistance occurs when bacteria develop the ability to survive exposure to antibiotics that were designed to kill them or stop their growth.
- Antibiotic resistance is a major obstacle in the treatment of infectious diseases caused by bacteria. Resistant bacteria can continue to grow, multiply and cause infection within the host, even when exposed to antibiotics.
- The result is that certain antibiotics can no longer be used to successfully treat certain infections.
- This significantly affects our ability to prevent and treat these diseases, increasing recovery time and the length of time that people stay in hospital. It can also lead to more people dying from infectious diseases.
- When this happens, it’s necessary for scientists to develop new antibiotics that the bacteria do not have resistance to.
How does antibiotic resistance occur?
- Understanding the mechanisms by which bacteria become resistant to antibiotics is a key task in preventing the development and spread of antibiotic resistant bacteria.
- Understanding these mechanisms will also be important in trying to prevent bacteria developing resistance to any new antibacterial treatments that may be produced in the future.
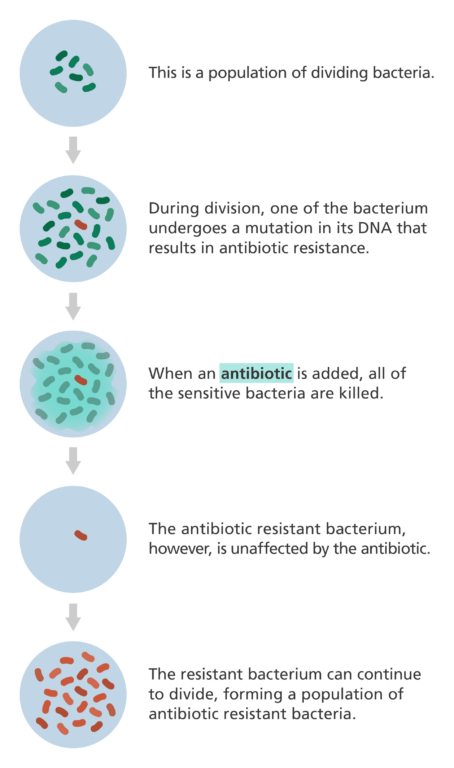
- Antibiotic resistance often occurs due to changes, known as mutations, in the DNA of the bacterial cell. It can also occur when resistance genes are passed between bacterial species, known as horizontal gene transfer.
- These changes enable the bacteria to survive the effects of antibiotics designed to kill them. For example, they might find ways to process the medicine so that it is no longer toxic or develop new ways to pump the medicine out of the bacterial cell.
- This means that when an antibiotic is used, all the bacteria that have not undergone a mutation are killed, while the antibiotic resistant bacteria remain unaffected.
- The antibiotic resistant bacteria can continue to divide and grow, producing even more bacteria that are not affected by the antibiotic.
- The existence of resistant strains of bacteria means that antibiotics or drugs designed to kill them no longer work, allowing them to spread rapidly, posing a risk to public health.
Why is antibiotic resistance on the rise?
- Antimicrobial and antibiotic resistance are serious, growing concerns in modern medicine.
- In fact, by 2050, scientists predict that the mortality rates for antimicrobial resistance could match those for cancer.
- A major cause of antibiotic resistance is people overusing antibiotics, for example when they are prescribed for minor conditions that would easily get better on their own.
- This is because overusing antibiotics puts evolutionary selection pressure on the bacteria, forcing them to evolve. This makes resistant strains emerging and spreading much more likely.
- Another cause of resistance is when patients don’t follow the course of antibiotics as prescribed by their doctor.
- To help prevent further emergence of antibiotic resistance, steps are being taken to ensure that antibiotics are only prescribed when there is a clear need for them and that they are used as directed by the doctor.