How is genomics being used to tackle Guinea worm disease?

The Guinea worm – also known as the little dragon, or Dracunculus medinensis – is a water-transmitted parasite that develops over a year in its host before painfully emerging from the skin.
This is part 4 in our series looking at how genomics is being used to tackle neglected tropical diseases. You might want to read part 1 first, here.
- Dracunculiasis, more commonly known Guinea worm disease, is a neglected tropical disease caused by the parasitic Guinea worm, Dracunculus medinensis.
- It is spread through stagnant water and can severely debilitate people for weeks and months.
- Great strides have been made to eradicate the disease: in the mid-1980s, there were 3.5 million cases worldwide. In 2020, that number had dropped to just 27.
Defeating the little dragon: tackling Guinea worm disease
Dracunculiasis, or Guinea worm disease, is the first disease caused by a eukaryotic pathogen to ever get close to being eradicated. In the mid-1980s, there were more than 3.5 million new cases recorded each year. This dropped to just 27 cases worldwide in 2020 – in Angola, Chad, Ethiopia, Mali, South Sudan and Cameroon.
This has all been done without the use of drugs or vaccines – but simply by controlling transmission. Recently, however, scientists have realised that eradicating the disease from humans is only one part of the story.
Genomics is now being called upon to aid the eradication effort.
Guinea worm disease can cause debilitating disability and bacterial infections that are hard to treat – increasing pain and disability associated with the disease.
Understanding the life cycle of the little dragon
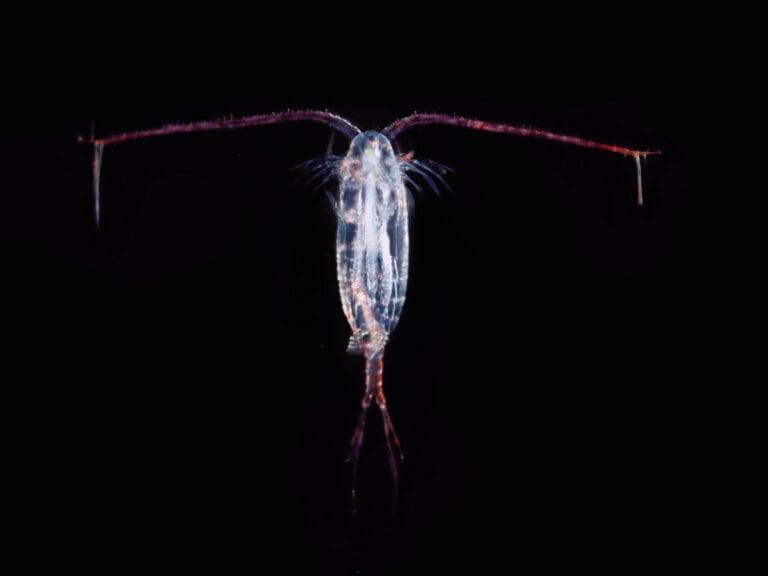
The Guinea worm affects communities by infecting fresh water relied upon for drinking. It starts its life cycle in fresh water, where it develops inside little water fleas called copepods. When people drink the contaminated water, they inadvertently take the copepods and Guinea worms into their bodies.
Once inside the stomach, the copepods are digested and the larvae are set free. They then move to the small intestine and penetrate the intestinal wall to enter the body cavity. Around 60-90 days later, the larvae mate and develop into adult worms – up to a metre in length and as wide as a piece of spaghetti.
Eventually, the larvae are released in milky-white liquid near the surface of the skin – usually on the leg or foot. This triggers an immune response in the host that results in the creation of an incredibly painful, burning blister on the skin – hence the name ‘little dragon’ – which bursts after about 24-72 hours.
The painful, burning blister compels individuals to immerse the affected limb in water – which is exactly what the worm wants, as contact with water releases many larvae back into the water supply.
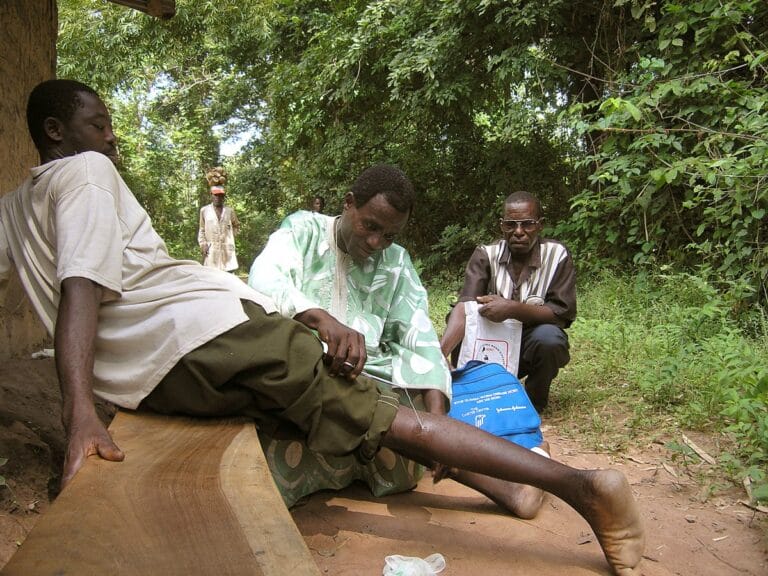
Extracting the worm from the skin
The best way to remove the worm from the body is for someone to slowly, painfully pull it out.
However, the worm is incredibly resistant to being removed. Over the course of several weeks the worm is pulled out and slowly wrapped around a stick, until it is released completely. If this process is carried out too quickly the worm can break and remain in the host, leading to further complications.
At this stage, and even after the worm has been removed, serious complications include major bacterial infections. In remote areas – where the worm is generally found – these infections can be very difficult to treat and can even sometimes be fatal.
Taming the dragon: blocking the transmission of the worm
One of the main reasons it has been possible to get so close to eradicating Guinea worm disease –but not for other parasitic diseases like malaria – is because the Guinea worm transmission cycle is relatively long at 12 months.
Providing communities with access to and information about the importance of clean water have also helped to block the cycle of transmission. This has included issuing water filters and pipe filters (personal filters that children can wear around their necks) to communities so they can easily filter their drinking water and avoid consuming the infected copepods.

Active surveillance…
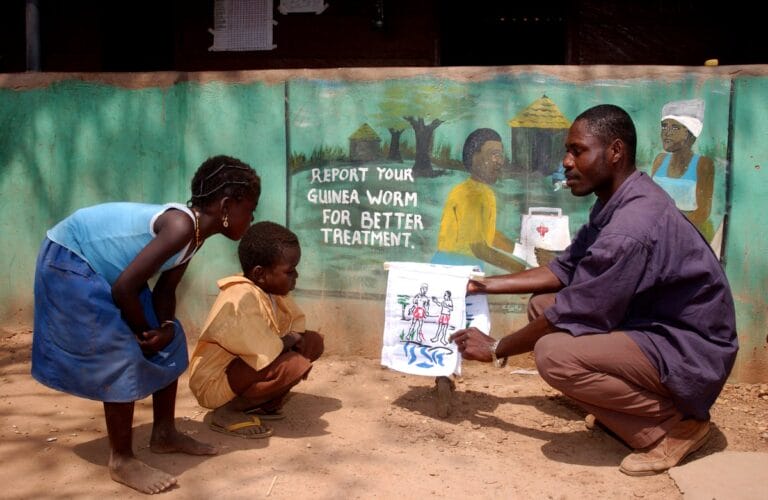
Active surveillance is also carried out in all countries that still have Guinea worm. This means that every time there is a case of an infection, an investigation is carried out to try to find out where the worm came from. This has helped to contain the disease and prevent further contamination of drinking water with parasite larvae.
This can be quite a challenge – not only because the worms take a year to grow to full size and emerge, but also because some communities migrate hundreds of miles every year or live in the middle of conflict zones.
…and confirmation of eradication
For a country to be certified as free of Guinea worm disease, it must have a robust and comprehensive surveillance system in place and be able to provide proof that there have been no cases of the disease for three consecutive years. This is the equivalent of three incubation periods for the Guinea worm.
The World Health Organization (WHO) then sends a team of experts to independently check the findings. If the necessary standards are met, they recommend to the International Commission for Certification of Dracunculiasis Eradication that the country is certified free of the parasite, who can then recommend that the country is declared free of Guinea worm disease.
Chad was thought to have completely eradicated Guinea worm disease as no cases were reported for 10 years – until new cases were reported in 2010.
Guinea worm disease in dogs: a new challenge?
Chad, in central Africa, reported zero cases of Guinea worm disease between 2000 and 2010. However, the WHO felt that the surveillance system used during that time hadn’t been rigorous enough – and Guinea worm disease was found once again in Chad in 2010.
Then in Chad in April 2012, Guinea worm disease was detected in dogs – increasing to 100 cases in 2014 and, in 2020, 1508 cases in dogs and 63 in cats. Research suggests that dogs cope with the worm better than humans, exhibiting a milder infection, less inflammation and making it easier to remove the worm.
The re-emergence of human infections in 2010, and the appearance of dog infections in Chad has raised several questions about the association between the infections in people and dogs. Do the dogs serve as a reservoir for human infections that are somehow spilling over into people? Or are the dogs infected with a different, distinct species of Dracunculus?
Are dogs spreading Guinea worm disease?
The concern is that infected dogs are driving the spread of Guinea worm.
But how do you stop a dog from drinking larvae-infested waters or releasing larvae into the water? To reduce the potential transmission of Guinea worm between dogs and human, new measures have been put into place, including:
- applying insecticide to water contaminated by dogs.
- offering a reward to people who notify authorities of dogs infected with Guinea worm.
- tethering of dogs with Guinea worm infections to keep them out of water sources.
Alternatively – are fish spreading Guinea worm disease?
What’s surprising about the 2010 human cases in Chad is that they didn’t have an obvious water source. In fact, cases were found outside of high-risk zones along the Chari River.
This raised the question: is there another host that might be channelling the infection to both dogs and people?
Freshwater animals – such as fish or even frogs – could be the cause. Fish are an important source of protein for people in Chad and surrounding areas. Although they aren’t actively infected by the disease, fish eat infected copepods and are often cooked by light smoking or drying out in the sun. Raw entrails are also often fed to dogs.
This could all enable Guinea worm larvae to survive and continue their life cycle in humans. Research is ongoing to test this theory, which could help find new ways to prevent the transmission.
How can genomics help?
The new cases of Guinea worm disease that emerged in Chad in 2010 were different to the previous cases. This adds a new challenge to the eradication campaign, suggesting we can’t rely just on reducing transmission.
Studying the genome of the worm could help provide more detailed insight into exactly why the disease has returned, so that interventions can be adjusted accordingly.
DNA sequencing: the key to success
Scientists released the first high-quality genome sequence of the Guinea worm in 2015, providing a valuable reference for further research.
Since then, researchers have used the sequence to answer important questions about the parasite. For example, in 2022, it was revealed that humans and dogs are infected with the same Dracunculus parasite – reinforcing the role of dogs in the persistence of Guinea worm disease in humans.
This information has confirmed there is a major animal component to the transmission of the Guinea worm, providing a much better understanding of how it spreads.
One way may be to design further interventions to prevent infection in dogs as well as any potential intermediate hosts, such as fish.
Defeating the little dragon
Impressive progress has been made against Guinea worm disease. The new cases in Chad and the transmission between dogs and humans pose new challenges – but with science, it’s likely that these are not insurmountable challenges.
Continually improving our understanding of the biology of the Guinea worm will help to strengthen efforts to eradicate the disease. New techniques in genomics and analysis of the Guinea worm genome are valuable tools to help solve this puzzle and find a way to block the way of the dragon.